Personalized care from hospital to home
Thrive offers an evidenced-based solution to address social determinants of health for people insured by Medicaid during the transition from hospital to home.

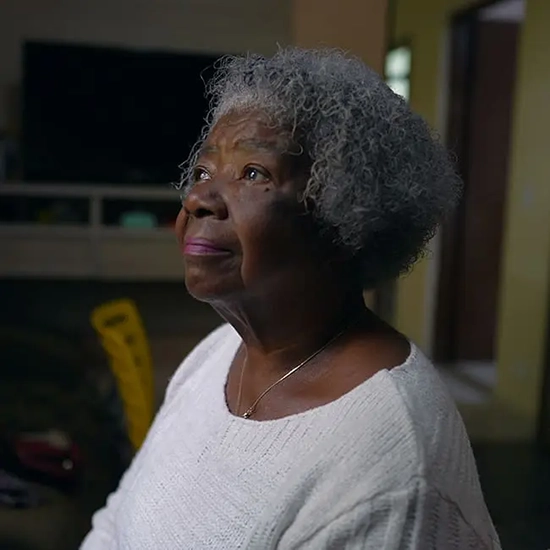
The transition home after a hospital stay can be overwhelming.
![]() Many people report being confused about medications, are unsure of instructions provided at discharge, and are unable to care for themselves.
Many people report being confused about medications, are unsure of instructions provided at discharge, and are unable to care for themselves.
![]() Others have difficulty with finances, transportation or housing, are unable to get to follow up medical appointments or have limited social support.
Others have difficulty with finances, transportation or housing, are unable to get to follow up medical appointments or have limited social support.
The period between a hospital stay and returning home is called a “care transition”.
According to research, poor care transitions are due to ineffective care coordination and poor communication between healthcare providers. Unaddressed health related social needs, known as the “social determinants of health”, are also linked to poor care transitions. These factors together, lead to increased hospital readmissions, poor outcomes, and decreased patient satisfaction.
People insured by Medicaid are at higher risk for experiencing a poorer quality care transition.
More
rehospitalizations
Preventable emergency
room visits
Longer wait times
for specialists
Difficulty accessing
primary care

Thrive offers an evidence-based solution to support people insured by Medicaid who have experienced a recent hospitalization by addressing social determinants of health.
Recent requirements from the Joint Commission and the Centers for Medicaid Services now require that hospitals collect information on social determinants of health and provide referrals to resources.
Our impact makes a difference:
“I add Thrive to a PMHH (home care) referral to help bolster the referral knowing that the patient receives an extra hand to help with situations that we sometimes over look or forget about. This might include picking up a medication from the pharmacy because the patient cannot get there or helping to set up the patient’s transport for an upcoming appointment.”
—Dianna McCollum, RN BSN
More than
clients have been served through our referrals.
“I feel helped. I feel heard. I feel seen.”
—A Thrive participant shares their experience

It’s not just enough that you were discharged from the hospital and you made it home, we want you to have a good recovery and that’s what it means to thrive.
—Margo Brooks Carthon, Executive Director of Thrive

How does Thrive work?
![]() Thrive virtual nurse case managers partner with the discharging medical and home care teams to address social and clinical needs following hospitalization.
Thrive virtual nurse case managers partner with the discharging medical and home care teams to address social and clinical needs following hospitalization.
![]() Our interdisciplinary team-based and embedded- community approach supports healing and recovery after hospitalization.
Our interdisciplinary team-based and embedded- community approach supports healing and recovery after hospitalization.
![]() Our proven track record of partnering with academic, clinical and community-based services has resulted in better outcomes post hospitalization including decreased Emergency Department use, increased patient satisfaction and improved quality of life after hospitalization.
Our proven track record of partnering with academic, clinical and community-based services has resulted in better outcomes post hospitalization including decreased Emergency Department use, increased patient satisfaction and improved quality of life after hospitalization.